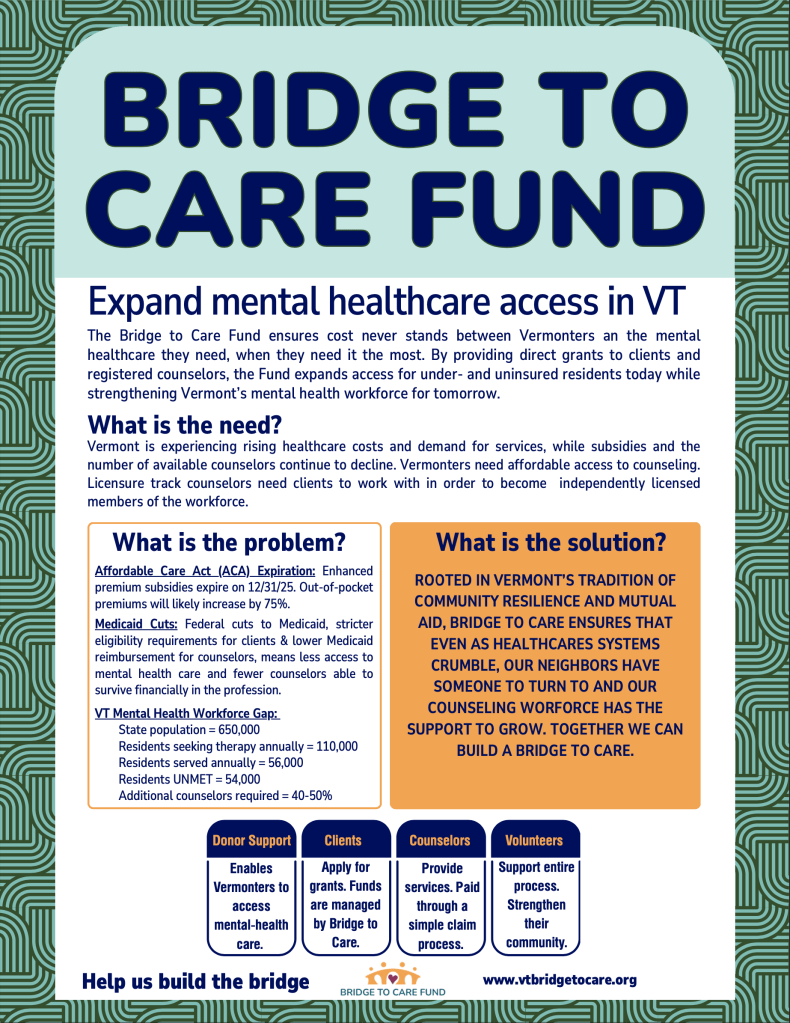
Vermont is experiencing an urgent crisis in access to mental health care. Each year only about half of Vermonters seeking care are able to connect with a clinician. The result is delayed or no treatment, increased emergency department use, higher acuity at intake, and preventable suffering. As federal policy shifts threaten the affordability of health coverage, and Medicare Advantage plans exit the state, thousands more Vermonters will lose access to care or face significant financial and geographic barriers to treatment.
The existing issues are on multiple fronts. Community mental-health agencies face difficulty retaining clinicians and stagnant reimbursement rates from insurance. Many private clinicians opt out of insurance altogether to remain financially viable and/or limit caseloads to manage burnout or diversify income. Pre-licensure clinicians in training face financial burdens and licensure hurdles. Vermont needs about 1,700 additional clinicians and without solutions the gap will widen. Bridge to Care exists to close this divide: funding direct access to care for underserved Vermonters while building the mental-health workforce that serves them.
Key federal pressures: what’s on the table
Expiration of the Affordable Care Act (ACA) enhanced subsidies on December 31, 2025.
- The extra ACA premium tax credits added during/after the COVID era (via ARPA, extended under IRA) are set to expire on December 31, 2025. (link)
- Without the enhanced credits, out of pocket expenses for premiums will increase up to 75%. (link)
- Millions of Americans are estimated to become uninsured or to have extremely high deductibles that will discourage them from seeking medical care. (link)
Implications for Vermonters
- Moderate and low-income Vermonters enrolled via the ACA marketplace will see substantial premium hikes.
- Some will drop coverage altogether due to financial hardship and go uninsured.
- The pool of insured will be reduced, which could worsen the “risk mix” for insurers (fewer healthier people), putting upward pressure on premiums and insurer stability.
- The state might face political pressure (and moral pressure) to step in with state-level subsidy programs, risk corridors, or affordability assistance to blunt the blow.
Proposed / enacted Medicaid cuts (“One Big Beautiful Bill” / H.R. 1 / reconciliation law)
There’s significant movement in Congress toward substantial cuts in federal Medicaid funding over the next decade. Some key points:
- The reconciliation legislation passed in 2025 includes major Medicaid reforms: stricter eligibility verification, new work/reporting requirements, constraints on state-directed payments, and provider tax limitations. KFF+7KFF+7Center for American Progress+7
- Some analyses estimate over $1 trillion in cuts to Medicaid over 2025–2034 under the law, and reductions of 10–15% (or more) in federal Medicaid support. Medicare Rights Center+7Center for American Progress+7KFF+7
- Rural hospitals and providers have warned that Medicaid cuts would particularly harm rural health infrastructure, because many rely disproportionately on Medicaid reimbursements to stay viable. Reuters+3American Hospital Association+3Harvard Chan School of Public Health+3
- Some states (especially Medicaid expansion states) may face pressure to scale back benefits, shrink provider payments, restrict eligibility, or shift costs to states. Center for American Progress+4Commonwealth Fund+4KFF+4
- The cuts also include changes in how states can use provider taxes or directed payments—tools many states use to support Medicaid funding flexibility. Center for American Progress+3KFF+3Center for American Progress+3
Implications (for Vermont):
- Vermont’s Medicaid program would come under pressure: the state may have to reduce benefits, cut provider rates, limit eligibility, or absorb more of the cost in its own budget.
- We have already seen a scaling back of services and closure of clinics in Vermont. In rural areas or smaller facilities, this strain will be amplified.
- Cuts will force Vermont to make additional trade-offs in reductions in access to care, provider reimbursements, or enrollment caps.
- Instability in Medicaid funding impacts Vermont’s ability to invest in insurance reforms, squelching innovation.
What this All means for Vermont
- Premium shock & coverage loss are almost certain in 2026 if Congress lets ACA enhanced tax credits expire. Vermont will see a sizable drop in marketplace participation unless the state steps in.
- Many Vermonters will go without insurance putting their health, lives, families and financial security at risk.
- Many Vermonters will suffer significant cost of living increases and quality of life impacts to meet high premiums and deductibles.
- Many Vermonters will not seek medical care due to extremely high deductibles.
- State-level relief becomes politically and fiscally necessary. Vermont may try to craft its own supplemental credits, reinsurance programs, or targeted subsidies to smooth the impact, but its fiscal capacity is very limited.
- Medicaid becomes a battleground line item. Rather than expansion and reform, pressure will mount cut services.
- Provider/health system stress accelerates. Financial stress for hospitals and providers will be magnified, especially for small, rural, or specialty practices. Vermonters will endure the strain of traveling farther for care, and remaining providers and facilities may be overwhelmed.
- Greater uncertainty and volatile transitions. Rather than smooth implementation of reform, the state’s efforts will be disrupted, or scaled back to protect foundational coverage and prevent provider collapse.
- Politics become fiercer. As coverage losses mount and premium spikes hit voters, pressure will intensify on Vermont’s state government to intervene. Expect more battles over state subsidy funding, Medicaid budget tradeoffs, and health reform roadmaps.
Vermont’s Mental Health Workforce Gap (2025–2027)
Although Vermont lists 3,836 active licensed mental-health clinicians, the functional clinical workforce—those available, full-time, and accepting insurance—covers barely half of the state’s current demand for outpatient therapy.
To achieve equitable, timely access (intake within 14 days statewide), Vermont would need an estimated +1,700 additional working clinicians or equivalent FTE capacity—about a 45 % expansion of its current mental-health workforce.
Current Situation
| Metric | 2025 Estimate |
| State population | 650,000 |
| Residents seeking therapy annually | ≈ 110,000 |
| Licensed allied clinicians (LCMHC, LICSW, LMFT, psychologist, etc.) | 3,836 |
| Average clinical FTE (after part-time, admin, supervision) | 0.7 |
| Effective clinical FTEs | 1,882 |
| Functional FTEs (after geographic, payer, specialty limits) | ≈ 940 |
| Clients served annually | ≈ 56,000 |
| Unmet clients / year | ≈ 54,000 |
| Additional clinicians required | ≈ 1,700 ( +45 % ) |
Why the Shortage Persists
- Low reimbursement & rate lag: Medicaid and commercial rates trail inflation by >30 %; Designated Agencies (DA) cannot compete with private-sector wages.
- High vacancy & burnout: 20–40 % clinician vacancy rates across Designated Agencies; turnover >25 %.
- Uneven distribution: Heavy concentration in Chittenden Co. and Montpelier corridor; rural counties underserved.
- Payer barriers: ~50 % of private practice clinicians are out-of-network or only accept private pay to make the career financially viable. This leaves many middle income, Medicaid and low-income clients without options.
- Workforce development: After 2 to 3 years of graduate school, including a typically unpaid 700 hr. internship, pre-licensure clinicians face the strain of doing 2-3 years of supervised practice while paying back student loans, paying for supervision, studying for board exams and meeting additional costs until they achieve licensure.
- Supervision bottleneck: Info on need for supervisors????
Regional & Specialty Gaps
| Area | Key Need |
| Northeast Kingdom, Islands, rural Bennington/Rutland | General outpatient, school-based, mobile crisis |
| Statewide children/adolescents | Child therapy, psychiatry, trauma specialization |
| Dual-diagnosis & SUD | Co-occurring expertise, residential beds |
| Medicaid network | Rate parity, streamlined credentialing |
What Would Close the Gap
| Lever | Approx. FTE Impact (by 2027) | Description |
| +10–15 % Medicaid rate increase | +250 FTE | Retains existing clinicians within DAs |
| Supervision-pipeline expansion | +150 FTE | Accelerated licensure & intern-to-rostered conversion |
| Loan-repayment / rural housing incentives | +200 FTE | Recruitment into shortage counties |
| Tele-behavioral infrastructure | +150 FTE | Extends urban clinician reach statewide |
Total recoverable capacity: ≈ 750 FTE ( ~ ¾ of the shortage )
Key Takeaway
Vermont’s mental-health shortage is due to a lack of funded, sustainable capacity.
Strategic investment in provider reimbursement, workforce pipelines, and tele-behavioral integration could eliminate the equivalent of a 54,000-person annual access gap by 2027. (check in on this number)
Strong communities care for one another. Right now, thousands of Vermonters are waiting months for the mental-health support they deserve. By donating, volunteering, or spreading the word, you help ensure that care is accessible, affordable, and close to home. Together, we build a healthier Vermont.